Did you know that point-of-care-ultrasound (POCUS) got its start with American military medicine?
Similar to the tech behind the internet, GPS, Siri and Alexa, POCUS emerged from the Defense Advanced Research Projects Agency (DARPA) with a mandate to arm military physicians with emergency ultrasound in caring for soldiers in 1991’s Operation Desert Storm.
It turns out our military veterans are also POCUS veterans, so we set out to honor them with a listening session on their most memorable POCUS moments — and how they’re using portable ultrasound in their daily practices.
We extend our deep gratitude to these professionals for their service and for their time in speaking with us.

The Versatility of Point-of-Care Ultrasound: Dr. Jon Monti
VITALS:
- US Army Major, Retired, 17 Years as Physician Assistant
- Bronze Star Medal with 3 Oak Leaf Clusters
- 2016 EMPA of the Year
- Emergency Medicine Fellowship
- Emergency Ultrasound Fellowship
- Society of Point-of-Care Ultrasound (SPOCUS)
BACKGROUND:
I was fortunate to be exposed to POCUS early in my career, working with and training under some pioneers in the field, and POCUS has figured prominently in my career, reinvigorating my passion for patient care.
First introduced to POCUS while deployed to a remote Afghan outpost in 2005, my team of four medics and myself supported a small surgical team and Special Forces personnel. The surgical team had the first portable US machine, the SonoSite 180, developed under DARPA.
I became fascinated with ultrasound’s utility in trauma and fell in love with its potential when I was able to employ it during a MASCAL event to accurately detect a traumatic pericardial effusion after simply reading the book and scanning my medics during the deployment.
HOW I USE POCUS IN MY WORK:
During my EMPA fellowship, I had the opportunity to design and execute research demonstrating that PAs, medics, and even a few Army cooks, were able to accurately detect pneumothorax with ultrasound after 10-minutes of training — and my co-author Rob Blankenship loves pointing out that the cooks performed the best in the study.
Since retiring from the military, much of my career has focused on similar research that demonstrates the ability of various non-physician clinicians, such as medics, to safely and accurately employ POCUS following focused training.
A decade ago, machine availability was the greatest barrier, but companies like Vave and others have done much to make ultrasound ubiquitous across the healthcare realm by making machines better, more versatile, and more affordable.
WHAT MOTIVATES AND INSPIRES ME:
In addition to research, I spend a lot of time training and educating clinicians — medics, medical and PA students, residents, and physicians. It is truly inspiring to see that light bulb turn on in their heads, whether it be from gaining a better understanding of the cardiac structure and function, or how POCUS could enhance the care they will, or already are, providing.
What most inspires me is how POCUS is such a versatile tool — research demonstrates that everyone from medics and nurses to PAs and physicians can be variably trained to safely and effectively utilize POCUS to enhance patient assessment and care.
Like most clinical skills, POCUS competency and expertise are less about clinical rank, title, or profession, and much more about quality of training, experience, deliberate practice, and dedication to lifelong learning.
And really, that’s what medicine is all about, finding the ways and means to provide the best care we can for those that need it most.
MY MOST MEMORABLE POCUS EXPERIENCES:
I used POCUS frequently during my deployments to assess trauma patients, musculoskeletal injuries, and to guide procedures. Operating in austere, resource-limited settings means that diagnostic and procedural adjuncts like x-ray, CT, and MRI are rarely available.
I truly believe the value of POCUS is inversely related to the resources available within a practice setting, which makes it a truly invaluable tool in the austere military environment.
That’s why something as portable and versatile as POCUS becomes increasingly valuable in the management and disposition of patients — where answering simple yes/no clinical questions can be the difference in whether we request a medical evacuation.
Unlike the civilian sector, military MEDEVACs may come with considerable risks. With a limited number of helicopters operating in extremely dangerous environments, you risk diverting them from other more seriously injured or ill patients, possibly in the middle of a firefight, putting the flight crew and the patient at considerable risk.
Unfortunately, the unavailability of training remains the biggest barrier to widespread POCUS use, and the onus now falls to POCUS leaders and educators to create quality, sustainable training that well-considers the users and the applications they are capable of performing.

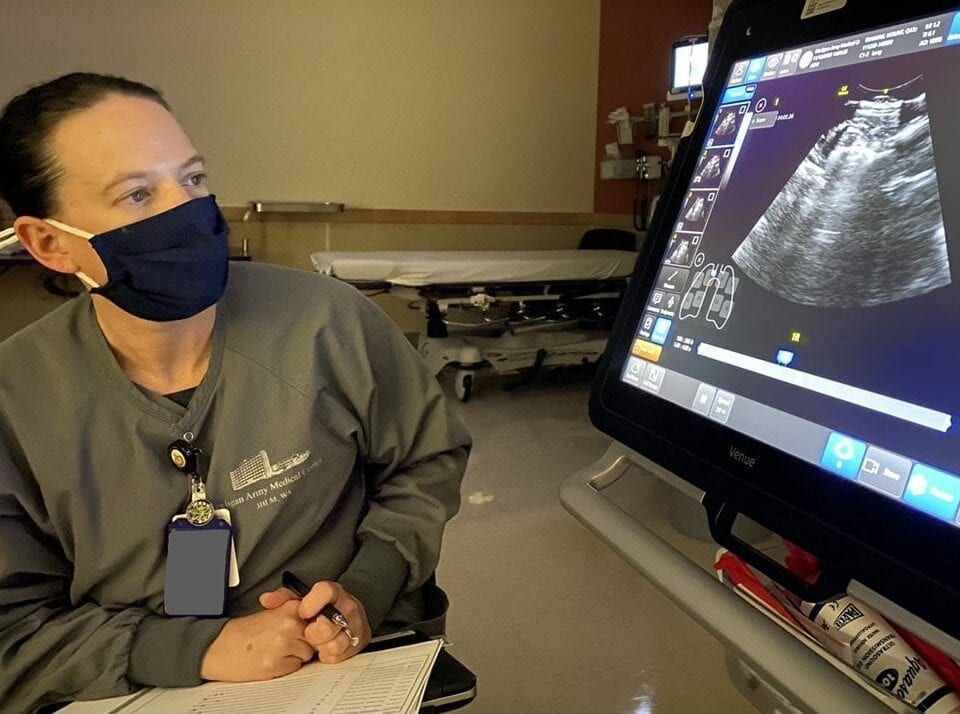
POCUS in the ICU & Emergency Medicine: Dr. Cristin Mount
VITALS:
- US Army Critical Care Physician, Academician, Administrative Leader
- Madigan Army Medical Center, Tacoma, WA
- Governor, Army Chapter, American College of Physicians
- 3rd Generation Service Member
- Wife of an Army Physician
- Mother of 3 Young Boys
BACKGROUND:
After med school at the Uniformed Services University of the Health Sciences in Bethesda, I did my Internal Medicine internship and residency at Madigan Army Medical Center in Tacoma. Following a Critical Care Fellowship at Walter Reed, I came back to Madigan where I started the Emergency Ultrasound Fellowship in the summer of 2020.
HOW I USE POCUS IN MY WORK:
Applications for POCUS cross the spectrum of military medicine — from daily use in the Emergency Department and ICU for quick clinical decision-making to aiding clinical decision-making and patient movement decisions in more austere environments.
It’s been amazing to watch POCUS technology evolve from the ancient machine I had as a resident (not good for much), to pocket-sized probes connected to a phone or tablet — putting ultrasound right at the point-of-care in a much easier, accessible way.
It’s been amazing to watch POCUS technology evolve from the ancient machine I had as a resident (not good for much), to pocket-sized probes connected to a phone or tablet — putting ultrasound right at the point-of-care in a much easier, accessible way.
WHAT MOTIVATES AND INSPIRES ME:
Helping create future generations of military medical practitioners is an awesome responsibility, and I’m motivated by caring for our country’s active duty service members, their beneficiaries and retired veterans — as well as the amazing medics, nurses and physicians I get to teach and train each day.
MY MOST MEMORABLE POCUS EXPERIENCES:
Most recently, I used POCUS in the ICU to help me decide against a risky patient transport and empiric therapy. The technology helped me eliminate the possibility from my differential diagnosis.
I greatly enjoyed the Emergency Ultrasound Fellowship, and I’m looking forward to expanding the infrastructure to support POCUS applications and education in the Army Internal Medicine community.

The stories from these veterans are touching, and inspiring.
Though they’ve highlighted the impact that point-of-care ultrasound has made on the lives of those tasked to protect and serve, they also have shown the range of impact POCUS has on each and every one of us.